Dakota State University, Madison Regional Health System, Global Polymer soar into action to protect area health workers
April 14, 2020
This paid piece is sponsored by Dakota State University.
Dakota State University faculty and staff, Madison citizens, Madison Regional Health System and Global Polymer have soared into action to address the critical need of area health care workers for personal protective equipment o defend against COVID-19 infection.
In recent weeks, DSU volunteers led by professor Justin Blessinger, director of the Mad Labs AdapT Lab for Accessibility Through Technology, came up with designs and then assembled over 100 face shields and about 20 of the 3D-printed respirator-type face masks.
Madison Regional Health staff have assisted in testing the prototypes and refining the designs. Blessinger connected with a local business, Global Polymer, which is ramping up to manufacture the most common-size mask with its plastic mold injection process. With the 3D printers available on campus, the DSU team is producing about 18 of the respirator-type masks a day. Shortly, Global Polymer likely will have the ability produce thousands of masks in a day, a much-needed exponential increase in production.
As reports of rising COVID-19 illness across the country started streaming in, along with distressing accounts of corresponding PPE shortages for medical professionals, Blessinger immediately began to think about how DSU might be able to help. He knew that some of the equipment in the AdapT Lab, as well as other resources on DSU’s campus, potentially could be used to make face masks and shields, both in short supply and critical for reducing transmission of COVID-19 disease.
He checked with area medical personnel, who confirmed that South Dakota medical professionals were indeed some of the ones being put in danger by the shortages. They also told him that face shields are as important as the respirator-type masks because they can be worn over the masks to offer additional protection against both spreading or contracting the illness. Also, the shields can be sanitized and reused many times more than masks, although after some number of uses they still do need to be replaced.
Blessinger had about 20 N95 respirators in his carpentry workbench at home. He thought about donating them to the Madison hospital but was concerned that the masks were too dusty because they had been in his shop for quite a while. However, indicative of how desperately hospitals need N95 masks, Madison Regional Health System happily took Blessinger’s donation, explaining also that they sanitize any PPE materials that come into the hospital.
Blessinger did what most researchers do when faced with a problem – he dove into finding out what information was available about the required specifications and possible processes for making shields and respirator-type face masks. He found out that the University of Wisconsin had researched the key protective components of face shields and then developed and shared plans on how to make them. Usually, the shields are made with commercially produced acetate sheets for the clear see-through front, but those supplies are hard to find, especially in the present crisis.
It occurred to Blessinger that before the days of computer projection and smartboards, teachers used overhead projectors that employed similar clear acetate sheets. The teachers could write or print on the clear film, lay it on the projector, and it would show up on a screen in front of the class. He thought it would be worth seeing if there were some lingering supplies in the community of those overhead projector sheets and if it would be possible to modify the UW design to make effective face shields with them.
A few social media posts and some phone calls later, Blessinger had a good supply of unused overhead projector acetates, quickly and generously provided by East River Electric, Madison Middle School, Madison High School and some DSU offices. Blessinger was still researching the specs and possible existing designs for also producing the 3D-printed filtration masks. So he put up a post on his Facebook page, asking if anyone would be willing to take over the work on the shields. He specifically asked if someone would be willing and available to create a prototype and, once approved by the hospital, dive into producing the shields.
Kathy Engbrecht, DSU instructor of computer science and retention specialist, volunteered to take on the shield design and production. She was able to redesign the shield so that it would work with the thinner overhead acetate material. Within a day, Engbrecht and Blessinger had a hospital-approved design and urgent requests from Madison Regional Health System for delivery of the shields as soon as they were completed.
Engbrecht, husband Doug and daughter Mandy – now home from USD because of the shift to online classees – sprang into action and created an assembly line, cutting the parts and constructing the shields. The first evening, they blasted through the supplies they had, completing 37 shields. The next day, they were able to get additional supplies and completed 62. After eventually finding more elastic for the headbands, the next day they were able to use the rest of their supplies to finish six more – for a total of 105 face shields.
Just like that, Madison Regional Health System staff had their much-needed protection, and community members can all breathe easier knowing that our medical professionals, many of them our friends and family members, have at least some of the PPE they need to stay safe and continue to be available to provide health care in the Madison area.
The University of Wisconsin had dropped from its posted design the cushioning foam strip across the forehead of the shields because of the difficulty of adequately sanitizing it. However, not having the foam strip makes the shield much more uncomfortable to wear.
The DSU designs for both the shields and the filtration masks use the inexpensive crushable adhesive-backed foam to improve wearability and effectiveness. Blessinger sought out DSU biology professor Michael Gaylor, who runs an extensive science lab at DSU, to see if he had any ideas about how to effectively sanitize foam without damaging it.
Gaylor actually had done some work on something similar as a graduate student, researching how to sanitize such materials through irradiating them. Those explorations are still in process, especially the possibility of someone purchasing a $3,500 irradiation chamber for the effort. The DSU team decided to go ahead with the foam band on both designs, given that comfort is important in ensuring that medical personnel continue to use the protection and because it is necessary to have an effective seal on the filtration masks.
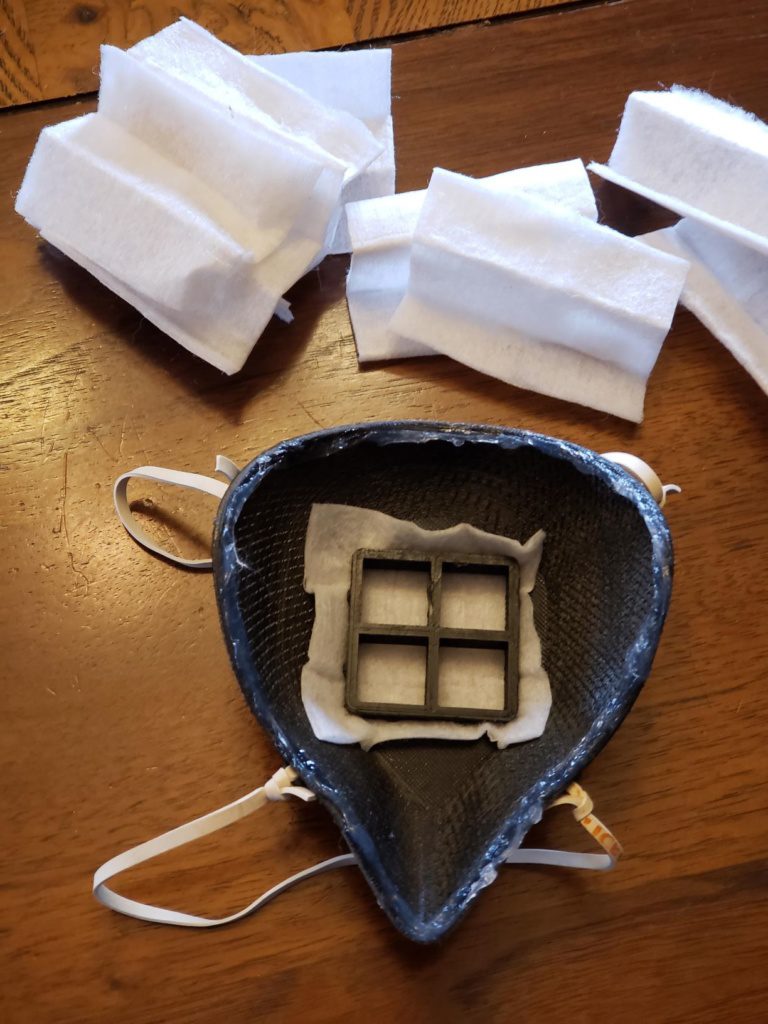
In the meantime, Blessinger continued on with his work, coming up with a reproducible design and process for producing filtration-type masks. As he said, “The 3D-printed masks have proven to be a much trickier path.” A few weeks ago, most of us didn’t know that there actually were many different types of medical face masks, and that one type – the N95 respirator mask – is the ideal one for those working in close contact with highly contagious patients. However, as we all have read in the media, there is a distressing shortage of N95 respirators in the U.S.
A difficult feature of N95 respirator masks is that to be effective they must fit tightly to the wearer’s face, not allowing even a microscopic virus to enter. Given the various sizes and shapes we all come in, this creates enormous challenges in the mass production of these masks. Blessinger found that a hospital in Billings, Mont., his home state, shared a plan using dental face-scanning technology to create masks perfectly shaped for one individual’s face shape.
Working from those plans, Blessinger and his colleagues figured out a way to produce more generic small- and medium-sized masks. As he said, “These masks are undoubtedly significantly better than surgical masks or the sewn cotton masks, but they aren’t a full replacement for N95 respirator masks, at least not yet.”
Madison Regional Health System told Blessinger that it had received a supply of sewn masks made and donated to the hospital by people in the Lake County area. These take care of some of the needs of personnel based on a reduced level of exposure. Therefore, the hospital asked the DSU team to do what they could to come as close as possible to something comparable to the N95 respirator masks.
Blessinger said: “That’s where things get harder. We have one promising prototype using an adhesive-backed, foam-rubber gasket inside the mask, and it reflects a prototype of a similar mask currently seeking N95-level air quality testing at Connecticut’s St. Vincent Hospital infectious disease unit. We’re watching St. Vincent’s research project closely for an update.” And once again, the foam is an issue for disinfection. It is one of the reasons why the commercial N95 masks have to be disposed of after a few uses, which is contributing to their short supply.
In the midst of all this, Blessinger knew that one of DSU’s 3D printers was not working correctly, and he was waiting on the delivery of another 3D printer for the AdapT Lab. He was concerned that the existing printer be ready to go the minute they had designs ready to try. Tom Halverson, DSU associate professor of computer science, and DSU Student Senate President Nathan Harmer came to the rescue. They spent several hours diagnosing the problem and, with some creativity, fixed the problem, upgraded the hardware and got the printer to Blessinger to work on at home. DSU staff also were able to check that the other available 3D printers were in good working order and they had the necessary supplies to print with. A few days later, the new AdapT Lab 3D printer arrived. Blessinger installed it alongside the other 3D printer in his basement, so he can continue to work from home as directed.
Blessinger was able to finalize a design, and the team started printing 3D masks. The design can use either pieces of HEPA-certified vacuum-cleaner bags as the filtration material or other medical filtration materials if they are available. The vacuum cleaner bags have proven to be only 2 percent less effective than the commercially – and minimally available – surgical filtration fabric. The vacuum cleaner bag material is thus not completely up to the N95 specifications, but again, it is far better than anything else medical personnel have available. Running the DSU 3D printers around the clock, the DSU teams can make about eight masks per day.
Blessinger reached out to Global Polymer about his work on the 3D masks. The company uses a proprietary molding process for ultra-high-molecular-weight polyethylene to produce specially designed, high-end plastic parts and is known for its skill and creativity in coming up with innovative solutions for challenging manufacturing problems.
Together, DSU and Global Polymer explored the possibility of going into larger scale production, with the manufacturer handling the production of the most-needed medium-size mask. Those without the industrial capacity of Global Polymer, like the DSU team, could focus on producing the more specialized small and large options. They even discussed how to produce the masks in a color-coded scheme, so it would be easy for medical professionals to grab the correct size. Global Polymer figured out it potentially oculd produce 400 masks a day, which would be a phenomenal boost to supply, especially for medical providers in smaller and rural areas in the Midwest.
Blessinger has contacted South Dakota state government about the possibility of large-scale production of the masks in Madison to help out but has not yet heard anything in response. In the meantime, Mike Whitehorn, Global Polymer’s mold design and CAD/CAM engineer, told Blessinger that the company is going to move forward and take the risk of the cost of making the molds to mass produce the masks because they’re such an important need in the community. Again, this is a wonderful example of a local business stepping forward to do what it can to address the needs of its community.
A major issue still is that of distribution – how to connect those who so desperately need PPE materials with those who can produce them. But as far as this project has come in less than a week, it is clear that when DSU and the extended Madison community rise up to solve a problem, the sky is the limit!
Kudos to everyone who has stepped forward to help out on this project, yet another example of how we are definitely: #DSUStrong #MadisonStrong #SouthDakotaStrong!